by Amanda Malachesky | Apr 14, 2017 | Brain Health, Functional Nutrition, Stress
Most of the clients that come through my doors have trouble sleeping. It’s one of the things I want to work really hard to help with right away, because sleep is so very important for restoring our health. How well we sleep affects our eating habits and metabolism (anyone out there trying to lose weight?), our moods, and our brain health and memory. Here are five reasons you may be having trouble sleeping, and how you can begin to help. Which ones speak to you?
1. Caffeine Consumption
A majority of my clients enjoy coffee and tea, and there is nothing inherently wrong with these beverages. In fact, they both contain food sources of antioxidants, which have a protective effect on our health. However, excessive caffeine consumption can definitely disrupt sleep in several ways. Of course the caffeine can keep you awake if you drink it too close to bedtime. What “too close” is varies greatly for people. For some, anything after first thing in the morning will keep them awake, while others can consume caffeine right up until bedtime without any perceived effect.
The other way that caffeine can influence your sleep is by its affect on blood sugar. For some people, the jolt of coffee really stimulates the body to produce energy. But with this stimulation, your body uses up your available blood sugar and can overshoot the mark, causing you to experience an energy slump later on in the morning or day. If you repeatedly reach for a caffeinated beverage to correct this problem, I hope you can visualize the roller coaster experience your body is riding to try to equalize your energy and blood sugar levels.
I generally recommend that you consume your caffeine before noon, and limit yourself to 1-2 cups of coffee or tea per day (not espresso!). Don’t forget that chocolate also contains caffeine, so you might want to rethink that flourless chocolate torte dessert after dinner.
2. Exercising Late in the Day
Exercise is an important part of any healthy lifestyle, but as with anything, too much of a good thing at the wrong time can cause trouble. Vigorous exercise, such as a cardio-type workout, is perceived by the body as a form of stress. In spite of the important cardiovascular effects, this stress elevates your levels of the hormone cortisol, which typically begins to decline after mid to late morning. If you exercise in the afternoon or evening, you may find that you have a difficult time falling asleep.
Aim to complete your exercise during the morning hours. The best for weight loss is on an empty stomach first thing in the morning, before you eat breakfast. An even better addition is to do your morning exercise outside in the daylight, as this helps reset your circadian rhythm, and can doubly help you feel more like sleeping when it’s time to go to bed.
3. Low Melatonin/Gut Infections
You may not be thinking about your melatonin levels, but being infected by hidden pathogens such as parasites, bacteria, or yeasts may have an impact on your ability to sleep well. There are several reasons this is so. Melatonin is a hormone that helps us feel sleepy. Some is produced by the pineal gland in the brain, but 70% of it is produced in the gastrointestinal system. When we have a pathogenic infection in the gut, one of the side effects of the infection can be a low level of melatonin. This can translate to more difficulty sleeping.
Gut infections also create elevated levels of cortisol, our stress hormone, which can also affect blood sugar levels. Cortisol is responsible for our circadian rhythm, and therefore has a lot to do with our wakefulness. Cortisol should be low at night when we are trying to sleep, but pathogenic infectious agents tend to create a rise in nighttime cortisol levels over normal, impacting our ability to go to sleep and stay asleep. If you suspect you may have a pathogenic infection, reach out to me or another practitioner who can help you explore this.
4. Staying Up Late (Even if We Sleep Longer in the Morning) and Not Getting Enough Sleep
Don’t lie, I know many of you burn your candle at both ends, and regularly stay up late. I used to be one of you! It’s not uncommon for people to go to bed at 11, 12 or even 1-2 am. I was guilty of this when my kids were little because I wanted just a little time to myself, and to catch up on things I couldn’t do while my kids were awake. I couldn’t have been more misguided about this.
Our brain needs to restore and repair itself while we sleep. For the best restorative effects, we need to spend time in REM sleep, dreaming. Because our sleep cycle is partially regulated by our cortisol rhythm, we naturally become sleepy in the middle evening, around 9 or 10 PM, and reach the point of lowest cortisol production in the middle of the night. We naturally begin to become progressively more wakeful later during the night.
When we push ourselves to stay up past that natural decline of cortisol in the evening, we get a second wind. Have you noticed this? Then we’re ready to stay up for a few more hours. But because of our cortisol rhythm, our deepest, most restorative REM sleep is available to us in the early hours of our sleep cycle, before midnight. Regularly going to bed before midnight generally leads to better overall sleep quality, and also helps increase the hours we are asleep.
You don’t have to look far for the benefits of getting enough quality sleep. People who sleep less than 6 hours per night are at an increased risk of infection, insulin resistance, obesity, diabetes, cardiovascular disease, cancer, arthritis, and mood disorders. Particularly interesting is the connection between sleep and blood sugar, insulin regulation, and obesity. Short sleep is associated with increased levels of the hormone ghrelin, and decreased levels of the hormone leptin. These two changes together are associated with increased appetite, and decreased satiety. Have you noticed that when you don’t sleep well, you are more hungry the following day?
This all adds up to the following recommendations: aim for about 8 hours of sleep, with a bedtime before midnight, ideally around 10:00 pm.
5. Blue Light and Screen Time
Finally, I want to discuss the effect of blue light screens, for example televisions and computer or tablet monitors, on our sleep. So many of us watch shows and movies at night, or surf the web to wind down at the end of the day. The blue light coming out of the screen suppresses your sleep hormone, melatonin. The easiest way to prevent this effect is to put away the tablet, and turn off the TV 2 hours before you go to bed. Use that time to unwind in a deeper way and prepare your body for sleep, by connecting with your family, reading a book, stretching, taking a bath, or some other calming ritual to help you settle down for the night.
If you can’t prevent screen time before bed, there are a few workarounds to reduce the impact of the blue light. There are several apps available that shift your screen to a more orange hue. This one, called f.lux is free. Some iPads have a function in the settings called Night Shift, which does the same thing. You can also purchase orange glasses, to wear while you work.
I do hope these tips can help get you sleeping longer and more deeply, so you are feeling happy, well-rested, and ready for your day. Let us know in the comments below if any of these tips has helped you.
by Amanda Malachesky | Apr 5, 2017 | Chronic Illness, Symptoms, Thyroid
The thyroid gland is a small, butterfly-shaped organ located in the neck. The thyroid is an endocrine gland, and is the primary gland that controls our body’s metabolic rate. Thyroid hormone is used by all organs and systems.
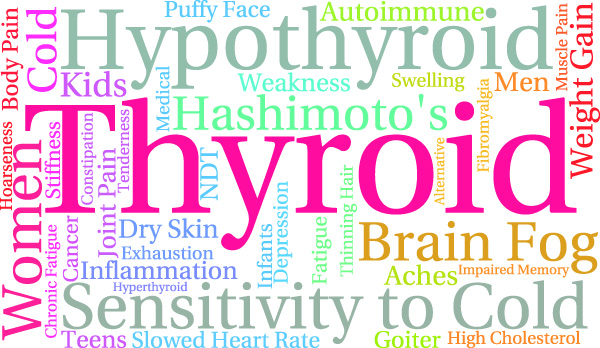
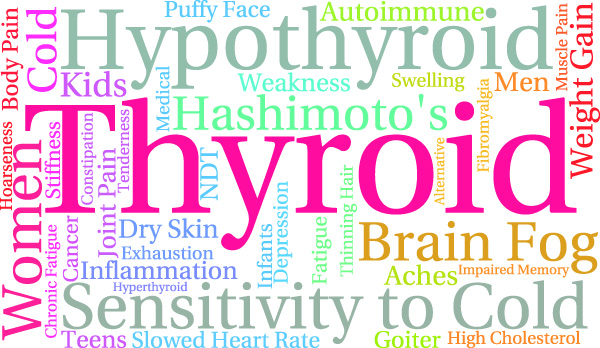
The Most Common Thyroid Symptoms Are:
- fatigue
- cold hands and feet
- hair loss
- constipation
- dry skin
- anxiety or depression, or manic cycling (from manic to depressive)
- poor wound healing
- infertility
- too many others to list here….
Thyroid problems are very common, and Synthroid, the synthetic thyroid replacement medication, is the third most common prescription in the U.S. Usually, the medication is prescribed after a blood test reveals high Thyroid Stimulating Hormone (TSH). However, Synthroid does nothing to address the underlying cause of the underactive thyroid gland.

Assessing the Thyroid
Thyroid hormone is created, released, transported, and used by a series of processes in the brain and body, and many things can disrupt the successful creation and conversion of thyroid hormone. A careful assessment of a complete thyroid blood panel is necessary to know where to direct action to correct a thyroid imbalance. This test includes:
- Thyroid Stimulating Hormone (TSH)
- Free T3
- Free T4
- T3
- T4
- rT3 (reverse T3)
- Thyroid antibodies: TPO and TG
Evaluating the TSH value, as is most commonly done, only tells us that the body is trying to produce more thyroid hormone to make up for a deficiency, but it doesn’t tell us WHY the body has too little thyroid hormone. If you suspect a thyroid condition, you may need to advocate for yourself with your doctor to run the whole panel. Evaluating the full panel allows a pracitioner to identify where the hormone is losing its effectiveness. For more information about how to interpret your thyroid labs, as well as lots of other thyroid resources, check out Stop the Thyroid Madness.
Thyroid Disruptors
Many factors can disrupt thyroid function. Stress can really disrupt thyroid function. When we are stressed, our body has elevated levels of a hormone called cortisol. Cortisol inhibits the production of Thyroid Stimulating Hormone (TSH), inhibits the body from converting T4 hormone (the transport form of thyroid hormone) into T3 hormone (the useable form of thyroid hormone), raises levels of rT3, which blocks the T3 receptor sites. Often, when stress is appropriately managed, and the adrenal system supported, thyroid levels return to normal. In this case, the thyroid dysfunction is a secondary problem.
Gut dysbiosis is another player in thyroid dysfunction. Some bacteria produce toxins, called Lipopolysaccharides, which decrease TSH AND disrupt the conversion of T4 to T3, while certain healthy bacteria assist with the successful conversion of certain intermediary forms of T3 into useable T3 hormone. Infection with pathogens can also impact the liver, as it tries to clean up their waste products, and T4 is converted into T3 in the liver. As with cortisol levels and stress above, when gut dysbiosis is corrected, by eliminating pathogens in the digestive system, thyroid symptoms often improve or disappear.
Problems can also occur at the cellular level: high stress, endotoxins (as mentioned above), systemic inflammation, and nutritional deficiencies can all disrupt the ability of cells to utilize the thyroid hormone at the cellular level. Addressing these kinds of root causes requires digestive function evaluation, nutrient status labs, and dietary and lifestyle modification.
Dietary choices can also have a huge impact on thyroid health, particularly with regards to autoimmune thyroid conditions. Testing for antibodies allows us to see whether the body is producing autoantibodies to thyroid tissue and damaging the thyroid gland. Antibodies will usually be elevated long before the organ has sustained permanent damage. Autoantibodies and autoimmune processes in general indicate that the digestive system needs support with it’s microbiome community, as well as the integrity of the barrier of the intestine. Consumption of certain foods, including gluten, diary, soy, and sugar are particularly damaging for those with autoimmune processes, which will be evident by checking for elevated TPO and TG antibody levels. If you’d like more information about how to get started avoiding these foods, click here to get a free recipe ebook by Dr. Izabella Wentz.
Help Your Thyroid Heal
A thyroid diagnosis doesn’t have to be a lifelong sentence to medication and feeling bad. Many people have been able to get into remission by addressing their gut health, adopting a thyroid-supportive diet and lifestyle, and for those that aren’t able to stop taking medication, using more bio-identical thyroid medications to provide more functional support.
If you know or suspect you have a thyroid condition, work with a functional health care practitioner who can help you fully evaluate your thyroid, test your gut for dysbiosis, and provide supportive dietary and lifestyle recommendations.
As a starting place for diet, you can explore and use the Autoimmune Paleo Diet. This diet removes foods that aggravate autoimmune conditions, and is anti-inflammatory. Changing your diet can be difficult, but it can also be the gateway to a positive change in your health. If you’d like to learn more about the Autoimmune Paleo Diet, Dr. Izabella Wentz, who recently released The Thyroid Secret film series, is offering a free, two-week cookbook and meal plan.
Click here to get your free copy.
The recipe book has 14-days-worth of delicious meal plans and recipes, including breakfast, lunch, dinner, and snack for two weeks. It also has a shopping list for each week, so that you can go to the store, stock up on everything you need and move on with your life.
If you would like support evaluating your thyroid, you can schedule a consultation with Amanda here.

by Amanda Malachesky | Feb 25, 2017 | Digestion, Functional Nutrition, Symptoms
So many of my clients suffer from heartburn, indigestion, belly aches, bloating, gas, constipation, or diarrhea. Are you one of them? I wouldn’t be surprised. Almost everyone has at least one of these symptoms on at least a semi-regular basis.
In particular, heartburn and reflux seem to be the most misunderstood of all. Heartburn is commonly thought, by doctors and regular people alike, to be caused by too much stomach acid. Common recommendations are antacids, and prescription PPIs (proton pump inhibitors), such as Prilosec.
But what would you say if I told you that heartburn is actually caused by too little stomach acid? Allow me to illuminate the physiology that explains why.
The stomach is designed to tolerate an extremely low pH of 1.0-1.5. It naturally creates hydrochloric acid when we begin to smell and think of eating, and while we eat our stomach with food. The hydrochloric acid has two functions: to chemically break down proteins into peptides, and to kill any incoming pathogens, such as unfriendly bacteria or parasites. It also facilitates absorption of vitamin B12 and iron. Vitamin B12 assists many essential processes in your body, and iron is important for energy levels. Do any of my readers out there have indigestion and fatigue?
The sphincter between the esophagus and the stomach (Lower Esophageal Sphincter or LES) maintains its normally-closed state by being exposed to adequate stomach acid. When stomach acid decreases, the LES becomes loose, and allows the acidic contents of the stomach to leak back into the esophagus. Because this material is quite acidic and because the esophagus isn’t designed to handle this acid, the sensitive skin there gets burned by the acid, and causes the familiar chest pain of heartburn.
The unfortunate truth about PPIs and antacids are that they are temporary fixes that may relieve immediate symptoms, but they do nothing to address the underlying cause of the heartburn, and further exacerbate the underlying cause: LOW stomach acid. Possible causes of low stomach acid include:
- Chronic stress
- Lack of pre-meal practices, such as preparing, smelling, and thinking about food (for example, eating convenience food on the run, in a hurry)
- Pathogenic infections
- Aging (we tend to produce less as we age)
- Hormone imbalances
- Consumption of coffee, chocolate, sugar, and alcohol can weaken the lower esophageal sphincter (LES), allowing heartburn to occur.
There are many other possible reasons why digestion may be compromised besides low stomach acid, such as inflammation from food sensitivities which can lead to malabsorption, slow motility, or small intestinal bacterial overgrowth (SIBO), which can lead to severe gas, bloating, and intolerance of certain foods, to name a few. But the phase of digestion that occurs in the stomach is one of the first major steps in the process, and when compromised, every step downstream is more of a challenge than it should be.
Here are some gentle, easy steps you can take to increase your stomach acid, improve digestion:
- Take a few minutes before your meals to look at, smell, and imagine eating your food, and express gratitude for your food, to stimulate saliva and hydrochloric acid secretion.
- Chew your food thoroughly, to help the acid you are making do its job more effectively.
- Consume some lemon or apple cider vinegar in water first thing in the morning, and before a high protein meal. Aim for 30 minutes before eating.
- If you suffer from heartburn and you consume coffee and/or alcohol, try eating some food first, to prevent weakening of the LES.
With these tips, I hope that you will find your digestion, energy, and elimination improving. Add a comment, and let me know if any of these tips made a difference for you.
by Amanda Malachesky | Jan 18, 2017 | Digestion, Functional Nutrition, Nutrition, Uncategorized

Are you thinking I’m talking about the difference between the Standard American Diet (SAD) and a plant-based diet?
Think again.
I have been a dedicated diet experimenter. Not a calorie-restriction dieter, but I have tried being vegan, vegetarian, pescatarian, mostly vegetarian with only familiar meat sources, gluten-free, sugar-free, paleo, keto, to name a few. I was trying all of these diets to try to improve my health problems, which in simple terms translated to hormone issues and fatigue. Some of them improved my health, and some quickly proved problematic.
While appropriate food is absolutely a crucial part of any healing protocol, understanding WHY you choose the foods you do is equally important. And if you are managing long-term symptoms or health problems, this is even more the case. Ultimately, there is no one right diet for everyone. Let me repeat: There is no one right diet for everyone! In other words, your food needs are very individual. Ignore this truth at your peril. Let’s dissect what I’m talking about here.
Quality Food, but Wrong Ratios
A few years ago, feeling bad in more ways than one, I stumbled across some information about the keto-adapted diet. I had already been eating a quality, low-processed-food, organic diet for many years, but I still had a dedication and practical addiction to eating carbohydrate-rich foods, including sugary treats. As long as they were gluten-free, we’re doing great, right?!
The keto dietary theory (and paleo theory, which overlaps in many ways) suggests that our bodies do not need to rely exclusively on glucose (sugar) to power our body, and that we can adapt to burning fat as ketones instead. In a keto diet, you eat a high fat, moderate protein, and low carb diet, which turns out to be absolutely delicious! Bacon, cream cheese, and butter are back on the menu, along with grass-fed meat and low carb vegetables. Grains, sugar, and high starch veggies are avoided, as are fruit, except for a small amount of berries. This diet works really well in a lot of cases to transform blood sugar, inflammation, and insulin issues, and reset metabolism. It often helps people lose weight.
When I found keto, I was ALL in! I had an extra fifteen pounds to lose, and hadn’t been feeling myself, and was sure that if I tried this, all my problems would be solved!
You can probably guess I’m going to suggest something different happened. I did feel good for a while, though not “amazing” as so many others advertised. I did lose the extra weight I didn’t want. But after about 8 months, my painful cycles turned to severely painful. I started sleeping even worse than I had been. And I had absolutely no energy. I could hardly get up off the couch, and folding my laundry had me needing a nap. What was going wrong??
In the end, it turns out that I wasn’t thinking about my health problems functionally. I didn’t consider the WHY behind the weight gain, or the hormonal symptoms I was having any farther than food. And because I wasn’t thinking in this way, the keto diet actually turned out to be the perfectly wrong solution. The dramatic increase in dairy consumption worsened my hormone symptoms, because dairy, even if it comes from dairies that don’t give supplemental hormones, comes from a lactating or pregnant animal. The low-carb aspect of the diet DID enable to me to break my addiction to carbs, but since my body wasn’t actually able to digest fats very well due to hidden infections I learned about much, the increased fat consumption worsened my digestion and acne, and left me without energy, and further stressed out my adrenal (stress response) system.
Basically, even though the diet I had been consuming before wasn’t great, it was holding together a pretty delicate system of adaptations to adversity in my body, and switching it up without laying a proper foundation had pretty dramatic and negative consequences. I got a “A” for effort, but an “F” for understanding the WHY behind my choices and what their effects would be. In short, I was asking the wrong questions.
Good Intentions, Accidental Consequences
After wondering why my acne was so bad, and my pain worse, and my digestion terrible, I decided to tilt things toward paleo. Add some more starchy vegetables, like sweet potatoes, and carrots, and squash back in, also some fruit, and lots of those yummy almond flour treats you read about on Pinterest!
My energy did improve a little with increased carbohydrate intake. But in spite of these good intentions, and thinking I was doing my immune system and inflammatory response a favor, I found my pain was still just as bad, there was no change in my skin, AND my digestion was even worse! So frustrating!
Enter oxalates. Oxalic acid is a naturally occurring substance found in humans, animals, and some plants. In plants, they are a defense mechanism, to dissuade herbivory. When consumed by humans, they are ordinarily broken down, bound to minerals, and excreted in the urine or stool. However, if a person has a permeable gut, and if that person is also deficient in minerals that bind to oxalates, they can enter the bloodstream, and travel anywhere the body, where they create sharp, jagged crystals that can cause joint and inflammatory pain.
It turns out that many of the foods that are very high in oxalates are also foods that are very commonly used in a paleo-type diet: spinach, chard, beets, sweet potatoes, plantains, almonds (and many other nuts), chocolate, and carob, to name a few.
Ultimately, even though these foods are healthy, and fine for many people, they can compromise others with certain physiological conditions, or make things far worse. Once again, I wasn’t considering the WHY about my symptoms and health issues, which was leading me down the wrong path. This is why it is so very important, if you want to use food as your medicine, to work with someone knowledgeable about food and how it affects the body, and to make choices aligned with where the body is at right now.
CAUTION: Do not go on a low-oxalate diet quickly! Consult with a knowledgeable practitioner to slowly work this into your dietary practice, to avoid painful symptoms!
How to Start Thinking Functionally About Food
Because we eat three or more times per day, it is crucially important to be choosing foods that will help your healing process. But how do you know which ones are right? We have to work carefully to find the foods that help, and identify the foods that trigger a problem. There are several ways to go about this. I’ll briefly describe two methods here: elimination diets, and food tracking. Food sensitivity testing is also an option, but because no lab test is perfect, an elimination diet is the gold standard for getting direct feedback about problem foods.
Elimination Diet:
In an elimination diet, you remove common problem foods, such as gluten, dairy, sugar, corn, soy, and eggs for a period of time, usually 2-3 weeks. Then, you carefully trial each food, one at a time, and only one per every 3-4 days, and observe to see if there are any negative consequences. You might be surprised about what causes a reaction, and the range of possible problems. Things like brain fog, achy joints, headaches, stomach aches, or gas might be some of the things that can happen. Once you are empowered with this information, the mysteriousness of some of these symptoms disappears and puts you back in the drivers seat of your life.
Food Tracking:
Food tracking involves journaling your food on a day-to-day basis for a while, noticing your macronutrient (protein, fat, and carbs) ratios, and noting any symptoms you feel, how your elimination patterns change or remain the same, and how your mood is faring, and seeing if you can correlate your responses to what you are eating. This kind of information also empowers you with the knowledge of what is creating an impact, and what is not, and provides focus on where to direct your attention to get the most benefit.
Download Your Food-Symptom Diary Here

by Amanda Malachesky | Jan 4, 2017 | Functional Medicine and Coaching, Functional Nutrition
When you decide you’re going to change something about your life, do you dive in and make drastic shifts all at once? Throw out half your pantry, or drive yourself to exercise obsessively, thinking that this approach will finally, once and for all, create the change you want to see?
While some of us are adept at altering our routines at the drop of a hat and maintaining those changes in the long term, most of us end up reverting to our previous habits within a few weeks. It’s easy to get started, because there is a rush of brain reward with something new and exciting, but when that wears off, we are left wondering what it’s for, and the old, comfortable habits start looking pretty inviting.
This is the scenario if you are going it alone. But when you add an observer, whether its someone you hire, a support group, or your best friend, and they are in on the project, your likelihood of success goes up dramatically. In coaching, we call this person an “accountability coach”, which is really just a fancy term for someone who holds you accountable to what you said you would do.
Furthermore, the changes you make are more likely to stick if you create just a few, actionable steps at a time. Think one to three new changes at a time. To create new, sustainable habits, we need time to try something new, adapt to the newness, and kind of “fake-it-till-we-make-it” until it becomes the new normal.
For example, if your goal is to eat healthier, you could just adopt a dietary theory that you think works. You could throw out all your sugar, chips, and soda, and go forward. But this is a very broad goal, and chances are, you won’t make it very far.
It is far more valuable to first get clear about WHAT you hope to accomplish with the change, and begin your process by imagining specifically how your life would be better if things were different. Once you’re clear on that, the necessary action steps become clear. You begin with a concrete action step like “Each time I want a soda, I will first drink a glass of water, and consider what else my body might be needing,” along with “I will eat sweet vegetables and foods like sweet potatoes, carrots, beets, winter squash, and whole grains regularly this week to crowd out sugar.” You begin creating a new habit without drastic measures. You create an enjoyable alternative, and observe. You encourage yourself to notice what happens. Your increase in sweet vegetables and grains might reduce your need for sugar, without a lot of fanfare and drama.
When you take on changes incrementally, you allow yourself to have a single-pointed focus, and really dedicate yourself to those one or two things that you think will make a difference. Trying to change too many things at once can be overwhelming, and lead to a feeling of hopelessness. Multi-tasking isn’t always better. When you approach making changes in this way, and you introduce something new and different every two weeks, as I have my clients do, within a period of months, you have developed many new habits over time. You might not notice how much has changed, until you look back and consider what things looked like in the beginning!
Through the twelve sessions of a six month program, my clients may have committed to a maximum of 36 goals through their program. That’s a lot of individual changes! Had I told them at the beginning that they would have given up sugar, lost pounds, resolved their sleep hygiene, created a weekly exercise routine, created stress-management strategies, increased the diversity of the vegetables and whole grains in their diets, and explored 10 new foods, they might not believe it! But this is really the secret: to make a big change, we start by taking on one thing at time, and doing it fully and well before we move on to the next thing.
Let me know below how you have manifested something big by taking small steps along the way.